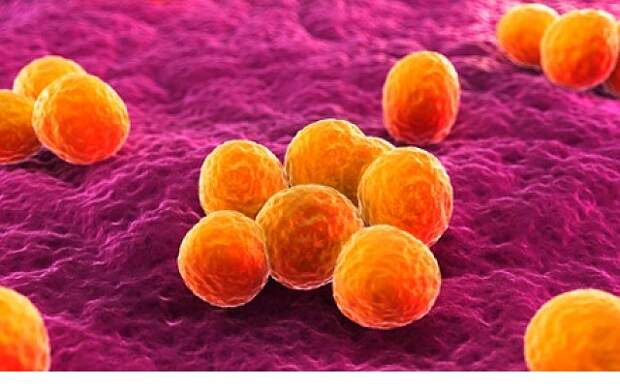
It was the initial sign of trouble. Three babies on the unique care ward at Rosie Hospital in Cambridge tested positive for the MRSA superbug. Fearing an outbreak of the risky organism, managers ordered a deep clean. Employees duly disinfected the ward and went back to work as typical. 4 days later the bug struck once more.
The circumstances, in 2011, prompted an investigation by the local infection handle team. By means of no fault of the staff, it left several queries dangling. Was it a new strain of MRSA (methicillin-resistant Staphylococcus aureus) or merely a cluster of unrelated MRSA infections? Had MRSA spread beyond the baby ward? And how had it come back?
What occurred subsequent was a exceptional feat of genetic sleuthing. A team of researchers, led by Sharon Peacock, a clinical microbiologist at the nearby Wellcome Trust Sanger Institute took up the investigation and sequenced the whole genomes of MRSA bugs taken from the babies. Regular genetic tests inspect only a handful of genes and are fine for confirming what strain is causing an infection. But with entire genome sequencing, scientists had the energy to reconstruct the history of each and every pathogen they identified.
The perform took time and effort, but it created clear what had occurred. First the team confirmed that it was an outbreak brought on by a new strain of MRSA. They then linked the outbreak to earlier infections on the ward and showed how it had spread to parents, including a mother whose child was on another ward. For their finale, they tracked down a health worker who unwittingly carried the bug and had reinfected the baby unit. The worker was treated for the infection and the outbreak was ultimately over.
As a demonstration of the energy of genetics, the intervention was dramatic. It was the very first time rapid genetic sequencing had been used to track and halt an outbreak. But the technology has considering the fact that moved on. Scientists at the newly formed Centre for Genomic Pathogen Surveillance at the Sanger Institute are establishing systems to track outbreaks of all sorts in close to genuine-time. It is not an overstatement to contact it a healthcare revolution.
“The outbreak in Cambridge, from the very first couple of babies becoming treated, to the identification of the wellness worker, took months of challenging work. The challenge now is to deliver true-time interpretation tools for hospital staff to spot outbreaks a great deal more rapidly,” mentioned David Aanensen, who is establishing the tools at the Sanger Institute. Employing the new technique, the hospital could have been on best of the outbreak in 3 days.
It will surely save lives. The Cambridge outbreak did not kill any person, but even as deaths from MRSA continue to fall, the infection nonetheless claims hundreds of lives every year in England and Wales. A different typical infection, Clostridium difficile, killed 1,646 men and women in the region in 2012. Other drug-resistant bugs are on the rise.
In a demonstration at his Cambridge workplace, Aanesen showed how the system works. If a hospital suspects an outbreak, medical doctors swab the individuals and send the samples for whole-genome sequencing. The business enterprise was after time-consuming and expensive, but Peacock’s investigation showed that the entire genome of a bacterium could be study in eight hours for less than £100. This price is set to fall much additional.
Aanenen’s demo program takes the genetic sequences and compares them with every single other and to DNA sequences held on a database. The laptop 1st searches a library of widespread mutations that make bugs resistant to drugs. It then compiles a list of antibiotics that will kill the strain in query and those drugs that will have no effect.
Next, the computer system builds up a household tree that shows how the bugs taken from each patient are associated to one particular a different and to other folks reported elsewhere. When the analysis is done, the info is beamed back to the hospital.
Armed with the benefits, medical doctors could go straight to the most productive drugs to treat their patients. That, at least, is the hope.
The loved ones tree is useful as well. It reveals when a string of infections belong to an outbreak brought on by a single strain that demands to be brought beneath manage. It can also assistance physicians trace the supply of an infection and warn them of any complications. For instance, a bug’s DNA may show that the strain is new to the UK, but brought on deaths in a hospital in Spain. A patient who visited the hospital on holiday may perhaps have carried the infection household with them.
Aanensen and his colleagues are demonstrating their method to researchers in the UK and Europe, exactly where speedy genome sequencing is progressively becoming offered. Addenbrookes Hospital in Cambridge is due to be the initially in the UK to adopt the method next year. The hospital’s infection control team will trial its use alongside tools that adhere to the movement of patients to track infections even extra closely.
Ultimately, the scientists want to do genuine-time, or close to true-time, tracking of ailments on a worldwide scale. But that will imply high-tech sequencing machines and infrastructure in other countries. “The concept is that this could be utilised by any laboratory anyplace in the planet,” said Aanensen. “We need to have to be hunting at South East Asia, South America and Africa. We will need to allow labs to do their own sequencing,” he stated.
By gathering information and facts on the newest outbreaks as they occur, the system should really choose up trends in drug resistance, for example by revealing the spread of recognized drug-resistant bugs, or the rise of bugs with new sorts of resistance.
One of the most critical emerging threats comes from carbapenemase-producing Enterobacteriaceae (CPE), a increasing household of drug-resistant bugs that infected only a handful of patients in England in 2006, but more than 600 in 2013.
Ross Fitzgerald at Edinburgh University’s Centre for Infectious Illnesses mentioned actual-time whole-genome sequencing of pathogens offers “enormous benefits” to hospital staff and sufferers, mainly because it can accurately predict which drugs will be powerful at containing outbreaks, but also reveal transmission routes within a hospital, the UK, and even on a worldwide scale. “This is a large deal. It is going to become routine and there are clearly important positive aspects for infection handle in hospitals,” he stated.